My son Anthony finds vest therapy the least favorite part of having cystic fibrosis. It’s understandable! Vest therapy helps the lungs and breathing by relieving mucous ingestion after a vigorous 30-minute lung workout.
Being shaken up rapidly for 30 minutes straight is not enjoyable. Anthony is ten years old and does the vest therapy twice daily.
Once in the morning and once at night. If he has a cold, he doesn’t do it four times daily, but that’s not so often, thankfully.
The therapy includes fun sensory activities I created for him. It helps him maintain healthy lung function and reduce phlegm that may cause breathing difficulties.
Inhaling Medical Solutions
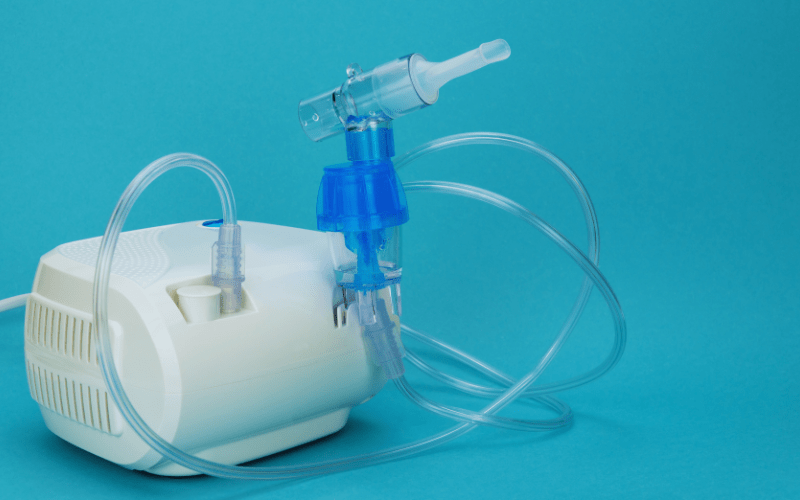
Anthony uses various treatments to help break down the mucus in his system.
He inhales solutions such as Pulmozyme and hypertonic saline solution daily. Anthony also takes Tobramycin on and off every 28 days, every 12 hours.
Additionally, Anthony uses Albuterol and Pulmicort (Budesonide) solutions as needed. Fortunately, he has no issues with taking these medications, and they help him cough up any phlegm.
Some people may wonder what he’s doing when he does his vest therapy. Seeing him stirred up like an ice cream shake in a blender is interesting.
Common Questions I Receive:

Anthony and my big Sister Magnolia are enjoying treatment time. He loves his aunty!
“The most common questions I receive from new parents of children with cystic fibrosis are about vest therapy.
They ask what it is, why it’s important, how it works, and what considerations they should consider for their child.
As someone who loves research, I thoroughly enjoy creating an informative post to address these questions and explain why vest therapy is crucial for cystic fibrosis patients.
Another common question I get is what came before vest therapy.
The answer is chest physical therapy, also known as CPT.
According to cff.org, “CPT is an airway clearance technique that involves clapping, vibration, deep breathing, and coughing to remove mucus from the lungs.”
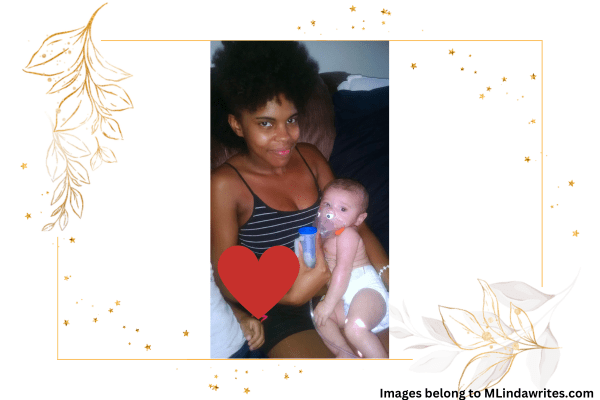
CPT Therapy for babies

Anthony and Mommy (Marlenny Linda). Anthony is two months old in this image.
These treatments were challenging to perform as Anthony grew older because he would not stay still, similar to Annie’s experience.
CPT therapy became a regular part of Anthony’s day. He received two treatments twice daily, each 15 minutes long, for 30 minutes.
However, when Anthony started crawling at around four and a half months, it became challenging to complete the therapy as he would move around a lot.
To make it easier, I started doing the therapy right before his nap time and bedtime as a routine after lavender baths.
T.V. and CPT Therapy
Doing treatment time together and watching Scooby Doo.
We used to watch Scooby-Doo together. While Anthony was distracted by Shaggy and Scooby’s antics, I would pat his sides and back.
I would save the front for last because he didn’t like it and would block me with his tiny hands, which was understandable.
Apart from helping his lung function, the added benefit was that the thumping and vibration helped him release his burps.
Though he never coughed out any phlegm or coughed at all, I made sure that it was a mandatory therapy to get done.
Fast Forward to age Three, the Beginning of Vest Therapy
Anthony is wearing his first smart vest, and his big brother Rudy is holding him.
We were excited about the intelligent vest as it meant that Chest Physical Therapy (CPT) would no longer be necessary.
However, Anthony was initially scared of the vest. He did not like the idea of connecting to a machine that would shake his upper torso for 15 minutes and vibrate his chest.
To help Anthony get used to the therapy, I started with small intervals of 2 to 3 minutes and congratulated him for completing each session.
Gradually, the duration of the therapy went up to 15 minutes, and Anthony became more comfortable with it.
Now, let’s get to the biscuits and gravy I mentioned earlier.
What is Vest Therapy, and why is it Important for Cystic Fibrosis?

Anthony, with his favorite Halloween sensory bin, I created using black beans and dollar store items.
Vest therapy, or high-frequency chest wall oscillation (HFCWO), is a standard respiratory treatment for managing cystic fibrosis (C.F.).
My son, Anthony, has been undergoing vest therapy for six years now, and he has adjusted pretty well to it.
I attribute this to the fun sensory activities I scheduled for him to keep him still or entertained during treatments, such as his favorite one, the Halloween bean bin.
Vest therapy helps to increase lung function in children with cystic fibrosis in two primary ways.
The first is through high-frequency chest wall oscillation, which involves vibrations.
The second is by allowing increased airflow to the lungs, facilitating the free flow of mucus.
What are the Mechanisms of Vest Therapy?

Anthony showed off his muscles while doing his nebulizer and vest therapy.
High-Frequency Chest Wall Oscillation:
- Vest therapy involves using an inflatable vest connected to a machine that generates oscillations.
- The rapidness of the vibrations is often too intolerable, which makes it necessary to take breaks often.
- These high-frequency vibrations are transmitted to the chest wall, helping to loosen and mobilize the mucus that accumulates in the airways.
- Anthony mentioned that after his therapy session, he could breathe better and feel more energized, often leading him to run around and stay active.
Increased Airflow:
- The oscillations generate a flow of air inside the lungs, facilitating the movement of mucus toward the more significant airways.
- This process is especially advantageous for people like Anthony, who suffers from C.F. Having CF causes mucus to be more dense and can cause blockage in the airways.
What are the Benefits of Vest Therapy for Cystic Fibrosis?

Mucus Clearance:
On the other hand, One of the primary challenges associated with cystic fibrosis in children is clearing their airways of sticky mucous.
The vest therapy is handy because it facilitates mucus clearance from the airways.
As children with cystic fibrosis grow older, the sticky mucous accumulates in their lungs. It can make breathing increasingly difficult for them, creating a frightening experience for parents.
However, the therapy helps break up the thick mucus in the lungs by applying vibrations to the chest wall. The vibrations make it easier to cough up and expel mucous.
Prevention of Airway Obstruction:
Vest therapy is essential to preventing airway blockage caused by mucus buildup.
This therapy helps mobilize the mucus and facilitates its removal from the lungs, making it easier for the lungs to perform the process.
The main goal is to assist the lungs in removing mucus, preventing complications such as infections or lung damage.
Improved Lung Function:
Regular vest therapy has proven to improve lung function in children and adults with cystic fibrosis.
Anthony maintains high lung function by being faithful to his vest therapy routine.
This therapy helps maintain optimal breathing, keeping his respiratory health in good shape.
Vest therapy allows individuals like Anthony to lead healthy lives by minimizing the impact of chronic lung disease associated with C.F.
Reduced Respiratory Infections:
- By promoting adequate mucus clearance, vest therapy can reduce the likelihood of respiratory infections.
Enhanced Quality of Life:
- Vest therapy plays a significant role in improving the overall quality of life for individuals with cystic fibrosis like Anthony.
- Maintaining clear airways helps alleviate symptoms such as coughing, shortness of breath, and fatigue, allowing individuals to engage in daily activities more comfortably.
Lastly, what considerations and best practices work well for your child?

My mom is holding Anthony and his favorite toy, snuggled in his blanket.
Individualized Treatment Plans:
The fantastic team at Nemours has set up a personalized Vest therapy for Anthony, which helps him improve his lung function and overall health.
Anthony’s smart vest machine undergoes annual inspections to ensure maximum airflow.
Anthony attends regular health checkups every three months so that his C.F. care team can evaluate whether the therapy needs to be adjusted or its duration changed.
Consistency and Adherence:
Thanks to Anthony’s consistent schedule, his lung function has not declined.
After completing his breathing examination, he showed no issues, letting the team know we were on top of our schedule.
The C.F. team wants to ensure regular mucus clearance and maintain respiratory health.
Monitoring and Adjustment:
Anthony’s healthcare providers at Nemours monitor his response to vest therapy and may adjust the treatment plan based on symptoms, lung function, or overall health changes.
To wrap it up,
Anthony and Mommy (Marlenny Linda) at Nemours Hospital in Lake Nona, Florida, for a check-up.
Vest therapy effectively manages cystic fibrosis by providing a unique way of clearing the airways. I am grateful that Anthony has his vest and can take control of his health by caring for his breathing and lungs.
Though some days may be more challenging, finding ways to make vest therapy time enjoyable can impact your child’s well-being.
Improving mucus clearance has boosted Anthony’s ability to stay active while preventing airway obstruction, which is crucial for maintaining respiratory health and is essential for children with cystic fibrosis.
Vest therapy plays a vital role in addressing the unique challenges associated with cystic fibrosis as part of a comprehensive treatment plan.
If you have a child with cystic fibrosis, I would love to hear about the techniques you use to make vest therapy more enjoyable.
Contact me with your CF stories!
You can tap the icons above and below and contact me through my Facebook, Twitter, LinkedIn, or Pinterest. I’ll happily hear about your success stories or provide tips!
Let’s continue breathing easier together, one treatment at a time. I used cff.org for my research. If you want to learn more about cystic fibrosis, please visit my linked websites.
You will find amazing facts and answers to common questions for children. You can also head to nemours.com to learn more about cystic fibrosis.
Marlenny Linda is more than just a writer; she's a passionate bilingual advocate for families with children with medical conditions. With a background in teaching English (TESOL/TEFL) and a Bachelor of Science in Liberal Arts, she crafts engaging, SEO-optimized content that informs, inspires, and connects with these families.
Her specialty is long-form content, where she dives deep into the topics that matter most, from navigating educational resources to fostering a fulfilling life for your child. Marlenny's innovative approach keeps audiences engaged and coming back for more.